Medical Treatment
Dr. Tasneem Nakhoda’s training in dermatology and plastic surgery allow her to treat all kinds of skin diseases. She uses a variety of lasers, topical solutions and oral medication to treat these conditions.
- Psoriasis
- Vitiligo
- Fungus
- Skin cancer
- Talengectasia
- Eczema
- Alopecia
- Herpes and other sexually transmitted diseases
- Hormonal problems
- Hyperhydrosis-excessive sweating
- Corns and callouses
- Ingrown nails and hair
- Spider Veins
- Acne Vulgaris

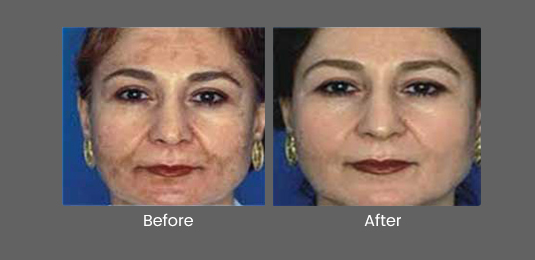
Pigmentation
Pigmentation can be treated in many different ways all-depending on the depth and the intensity of the pigmentation. The most common Asian pigmentation problem is melasma. The backbone of treating melasma is still sun blocks, skin lightening creams, and anti-oxidants but at Dr. Nakhoda`s SKIN INSTITUTE, we are equipped to treat more resistant pigmentation.
At the clinic you could be offered Mesotherapy with the U-255 Mesotherapy Gun, Revlite the state of the art Q switched Nd-YAG Laser or the new Spectra XT. Pigment not responding to the 1064 Nd:YAG laser can be treated with V-beam Perfecta (pulse dye laser). The pigmented lesions treated with the above lasers are Age Spots, lentigenes, Café-au-lait spots and Naevus of Ota.
Active Acne and Acne Scars
We treat active acne using a variety of lasers, oral medications and topical creams. We will understand your full medical history, examine your skin and prescribe you hormonal tests before we can decide what kind of treatment will be the most beneficial for you.
Acne Scar treatment is focused at removing scar pigmentation and returning the skin back to its smooth texture and surface.
Some of the lasers that might be adjunct to your treatment would consist of:
- Candela’s V Beam Perfecta
- Scarlet RF
- Lutronic’s eC02+ Laser Peel
- Lutronic’s Spectra-Spectra Pee
- Healite II™ (bluelight)
- Hydrafacial MD®
- Dermapen™
- Prizmah’s PRP
- Subscision

Removal of Birth Marks, Moles and Warts
There are many different kinds of birthmarks on the face and we are one of the first skin care clinics to non-surgically remove them.
If you have a red birthmark (Port-wine Stain) we would use the world renowned V-Beam Laser made by Candela, as it is the world Gold Standard for red birthmarks and other red colored growths such as rosacea and red scars.
If you want to remove a black, brown or grey birth mark (Nevus of Ota & Nevus of Ito) we will use Hoya ConBio’s Revlite and Lutronic’s Spectra
Warts can be removed with cryosurgery after close examination.

Frequently Asked Questions
What causes acne?
The causes of acne are linked to the changes that take place as young people mature from childhood to adolescence (puberty). The hormones that cause physical maturation also cause the sebaceous(oil) glands of the skin to produce more sebum (oil). During puberty, the cells of the skin that line the follicle begin to shed more rapidly. In people who develop acne, cells shed and stick together more so than in people who do not develop acne. When cells mix with the increased amount of sebum being produced, they can plug the opening of the follicle. Meanwhile, the sebaceous glands continue to produce sebum, and the follicle swells up with sebum. In addition, a normal skin bacteria called P. acnes, begins to multiply rapidly in the clogged hair follicle. In the process, these bacteria produce irritating substances that can cause inflammation. Sometimes, the wall of the follicle bursts, spreading inflammation to the surrounding skin. This is the process by which acne lesions, from blackheads to pimples to nodules, are formed.
I wash my face several times a day. Why do I still get acne?
Many people still believe that acne is caused by dirty skin. The truth is, washing alone will not clear up or prevent acne. Washing does, however, help remove excess surface oils and dead skin cells. Many people use all kinds of products, including alcohol-based cleansers, and scrub vigorously, only to irritate the skin further and worsen their acne. Washing the skin twice a day gently with water and a mild soap is usually all that is required.
Does stress cause acne?
Stress is commonly blamed for the development of acne. Stress can have many physiologic effects on the body, including changes in hormones that may theoretically lead to acne. In some cases the stress may actually be caused by the acne lesions, not the other way around! If the acne is being treated effectively, stress is not likely to have much impact on the majority of people.
I never had acne as a teenager. Why am I now getting acne as an adult?
Usually, acne begins at puberty and is gone by the early 20s. In some cases, acne may persist into adulthood. Such types of acne include severe forms that affect the body as well as the face (which afflict males more than females) and acne associated with the menstrual cycle in women. In other cases, acne may not present itself until adulthood. Such acne is more likely to affect females than males. There are several reasons for this. As females get older, the pattern of changes in hormones may itself change, disposing sebaceous glands to develop acne. Ovarian cysts and pregnancy may also cause hormonal changes that lead to acne. Some women get acne when they discontinue birth control pills that have been keeping acne at bay. Sometimes young women may wear cosmetics that are comedogenic-that is, they can set up conditions that cause comedones to form.
What role does diet play in acne?
Acne is not caused by food. Following a strict diet will not, clear your skin. While some people feel that their acne is aggravated by certain foods, particularly chocolate, colas, peanuts, shellfish and some fatty foods, there is no scientific evidence that suggests food causes or influences acne. Avoid any foods which seem to worsen your acne and, for your overall health, eat a balanced diet, but the diet shouldn't really matter if the acne is being appropriately treated.
Does the sun help acne?
Many patients feel that sunlight improves their acne lesions and go to great lengths to find sources of ultraviolet light. There is no proven effect of sunlight on acne. In addition, ultraviolet light in sunlight increases the risk of skin cancer and early aging of the skin. It is, therefore, not a recommended technique of acne management, especially since there are many other proven forms of treatment for acne. Moreover, many acne treatments increase the skin's sensitivity to ultraviolet light, making the risk of ultraviolet light exposure all the worse.
What is the best way to treat acne?
Everyone's acne must be treated individually. If you have not been able to control or reduce it immediately consult a dermatologist. Your dermatologist will decide which treatments are best for you.
What kind of cosmetics and cleansers can an acne patient use?
Look for "noncomedogenic" cosmetics and toiletries. These products have been formulated so that they will not cause acne. Some acne medications cause irritation or pronounced dryness particularly during the early weeks of therapy, and some cosmetics and cleansers can actually worsen this effect. The choice of cosmetics and cleansers should be made by your dermatologist. Heavy foundation makeup should be avoided. Most acne patients should select powder blushes and eye shadow over cream products because they are less irritating and noncomedogenic. Camouflaging techniques can be used effectively by applying a green undercover cosmetic over red acne lesions to promote color blending.
Is it harmful to squeeze my blemishes?
Yes. In general, acne lesions should not be picked or squeezed by the patient. In particular, inflammatory acne lesions should never be squeezed. Squeezing forces infected material deeper into the skin, causing additional inflammation and possible scarring.
Can anything be done about scarring caused by acne?
Scarring is best prevented by getting rid of the acne. Dermatologists can use various methods to improve the scarring caused by acne. The treatment must always be individualized for the specific patient. Chemical peels may be used in some patients, while dermabrasion or laser abrasion may benefit others. It is important that the acne be well controlled before any procedure is used to alleviate scarring.
How long before I see a visible result from using my acne medication?
The time for improvement depends upon the product being used, but in almost all cases it is more a matter of weeks or months instead of days. Most dermatologists would recommend the use of a medication or combination of medications daily for 4 to 8 weeks before they would change the treatment. It is very important for patients to be aware of this time frame so they do not become discouraged and discontinue their medications. Conversely, if you see no change whatsoever, you might want to check with your dermatologist regarding the need to change treatments.
Would using my medication more frequently than prescribed speed up the clearing of my acne?
Always use your medication exactly as your dermatologist instructed. Using topical medications more often than prescribed may actually induce more irritation of the skin, redness and follicular plugging, which can delay clearing time. If oral medications are taken more frequently than prescribed, they won't work any better, but there is a greater chance of side effects.
My topical treatment seems to work on the spots I treat, but I keep getting new acne blemishes. What should I do?
Topical acne medications are supposed to be used on all acne-prone areas, not just individual lesions. Part of the goal is to treat the skin before lesions can form and to prevent formation, not just to treat existing lesions. Patients are generally advised to treat all of the areas (forehead, cheeks, chin and nose) that tend to break out rather than just individual lesions.
My face is clear! Can I stop taking my medication now?
If your dermatologist says you can stop, then stop--but follow your dermatologist's instructions. Many times patients will stop their medication suddenly only to have their acne flare up several weeks later. If you are using multiple products, it may be advisable to discontinue one medication at a time and judge results before discontinuing them all at once. Ask your dermatologist before you stop using any of your medications.
Does it matter what time I use my medication?
Check with your dermatologist. If you were taking one dose a day of an antibiotic, you could probably take it in the morning, at midday or in the evening, although you should pick one time of day and stay with it throughout your treatment. With oral medications prescribed twice a day or three times a day, you should try your best to spread out the doses evenly. Some antibiotics should be taken on an empty or nearly empty stomach. For optimal results with topical treatments, you should strictly follow your dermatologist's recommendations. For example, if instructed to apply benzoyl peroxide in the morning and a topical retinoid at bedtime, it is important to follow these directions strictly. If the two were applied together at bedtime, for example, you could decrease the efficacy of the treatment because of chemical reactions that make them less effective.
I have trouble remembering to take my oral medication every day. What's a good way to remember? What should I do if I forget a dose?
This is a common problem. Many patients try to associate taking their medication with a routine daily event such as brushing teeth or applying makeup. It also helps to keep the medication close to the area where the reminder activity is carried out. In most cases, if you miss a day of your oral treatment, do not double up the next day; rather, get back to your daily regimen as soon as possible--but there may be different instructions for different oral medications. Ask your dermatologist about what to do if you miss a dose of your particular medication.